Gluten Intolerance – Increasing Awareness (even of your Dr.)!

Those Diagnosed & Undiagnosed – Both Need Help
I mention both those who are diagnosed as well as those who aren’t because:
1. Too often, even those who have received a diagnosis and are avoiding gluten continue to struggle with poor health. For them, we focus on the treatment of the secondary effects of gluten.
Why? Because complete normalization of gut lesions is very rare in adult patients with Celiac Disease – only 8% completely heal. [Reference cited at the end of this post.]
We have found that to restore the gut to a healthy, “non-leaky” state requires evaluation for the presence of:
• inhospitable organisms
• imbalanced probiotics (the good guys of the gut)
• other cross-reactive foods that mimic gluten without being gluten
• nutritional deficiencies
• hormonal imbalance, and more.
2. Of course with only 5% of our celiacs ever receiving a diagnosis and, at best, 1 or 2% of those suffering from gluten sensitivity ever getting diagnosed, we obviously have a lot of work to do.
Due to the fact that the majority of my time is spent in this area, I forget sometimes how current our knowledge base is here at the clinic. I find myself being surprised when I discover what other clinicians are saying to their patients.
An Elderly Woman Misdiagnosed
Let me give you an example: I lecture frequently at local Silicon Valley corporations. I am also a guest lecturer for several local Whole Foods. Two evenings ago at the end of a lecture about gluten intolerance, an elderly woman came up to me with lab results in hand. She was very sweet but didn’t look at all well.
I cannot diagnose someone without a prior examination and I was just about to tell her that when she began to speak. She had pictures of her colon as well as the doctor’s evaluation of the test that was performed to view her intestines. It said she had complete villous atrophy (the hallmark of celiac disease) and the pictures made that diagnosis very clear. I asked her what her doctor told her to do. She said that he diagnosed her with irritable bowel syndrome. This too was written on the report.
Trying to be diplomatic I asked if there was any mention of celiac disease. She looked at me sadly and said that she had asked about it specifically since it ran in her family but the doctor said that she was fine to eat gluten – and she was. Wow! It is difficult to fathom what the gastroenterologist was thinking when he wrote that report. I’m the first to give intestinal biopsies a hard time due to their insensitivity, but with complete villous atrophy (severe intestinal destruction) clearly evident, not to mention a strong family, one has to wonder.
While the patient only showed me the endoscopy report, I am curious to know if any celiac blood tests were performed. Did they consider she was perhaps too elderly to change her diet? My own mother didn’t go gluten-free until she was in her 70s and she is now 88. She states that her 70s and 80s have been the healthiest decades of her life! Such misdiagnoses occur quite commonly in our country, much to my dismay. And that’s focusing on celiac disease. What about gluten sensitivity; a condition that most clinicians don’t even know exists? How often do you suppose that is misdiagnosed?
What Are Some Common Misconceptions?
1. If a person doesn’t have celiac disease then they don’t need to remove gluten from their diet
2. The gold standard test for celiac disease diagnosis is an intestinal biopsy. If that is negative, there is no need for a gluten-free diet, regardless of blood testing or symptoms.
3. If their lab tests are negative (for either celiac or gluten sensitivity) then they are fine to continue eating gluten.
4. If a person has no digestive complaints and/or is not underweight, there is no reason to test them for gluten intolerance.
What is the Truth
1. If a person doesn’t have celiac disease, that doesn’t mean that they are not gluten sensitive. Gluten sensitivity affects a minimum of 10 times the number of people who have celiac disease. A conservative estimate puts that at 20 million Americans suffering from gluten sensitivity.
Considering it is known to decrease life expectancy, it is vital that we not miss the diagnosis of either of these debilitating conditions.
2. An intestinal biopsy is not a sensitive test. It requires marked damage to the small intestine before it shows positive. Dr. Fasano, one of the leaders in celiac research, has stated quite recently that he too no longer considers it the gold standard; not even close.
3. Even with the recent improvement of lab tests, we still suffer from a lack of sensitivity. The newest tests are a leap forward, but what really is the gold standard?
Many of us feel that it is embarking on a 30-day gluten-free diet. One must be 100% gluten-free for this to work – no cheating.
When done correctly, this free home test can very clearly tell you what your body thinks about gluten.
4. All too often, doctors are locked into the notion that an individual with celiac disease will present with severe digestive problems. While that certainly can be the case, more often the individual has mild or absent digestive problems but instead complains of skin problems, fatigue, depression, migraines, or joint pain, to name but a few.
It is truly maddening to hear that a doctor refused to test a patient solely because they did not have digestive problems or they were overweight – another misconception.
While we obviously have a lot more work to do, on the upside, it is wonderful to see that the leading researchers in the field now concur that gluten sensitivity is a very real condition that must be better understood. And to that end, many are devoting time and money to its research.
It is gratifying to see this as we have been witnessing the effects of gluten intolerance (both celiac disease and gluten sensitivity) in our practice for over 15 years. This is hopefully the beginning of widespread knowledge and awareness on the topic and that is exciting. In the meantime we still have a grassroots movement to keep going, so please continue to educate your friends and family.
Help to Increase Doctor Awareness
What can you do to increase the awareness of your doctor? There is now an amazing tool courtesy of the National Foundation for Celiac Awareness (NFCA). The NFCA has been tireless in their pursuit of increasing the rate of diagnosis of celiac disease. They are committed to the same increased awareness that we are.
Their President, Alice Bast, herself a celiac, is an amazing leader in this community and I am proud to have her as a friend. In a stroke of brilliance, Alice and her team recently created a tool for doctors that is easy, free, and will increase their awareness of gluten intolerance dramatically.
Per the NFCA: “Physician awareness in the U.S. has frequently been identified as a critically important yet unmet need – until now.” The program is called: Primary Care CME: Defining, Diagnosing, and Managing Celiac Disease. [CME stands for continuing medical education – doctors are required to attend continuing education seminars on an annual basis] “This program delivers the education to primary care providers, a community on the frontline of diagnosis, critically need.
It is also a resource for patients. Tell your doctor. He or she can get more information about this free program here: www.CeliacCMECentral.com. Per the NFCA: “Physician awareness in the U.S. has frequently been identified as a critically important yet unmet need – until now.” I hope you find this helpful. Please send me any questions you may have in the areas of gluten intolerance or clinical nutrition. As a destination clinic, we see patients from across the country as well as internationally. We are truly here to help you, your family, and friends.
Do you need help with your health?
We have the diagnostic and testing tools, the clinical experience, and a different medical approach to discovering the root cause of why you have the symptoms that are bothering you. As long as you are ready to make some dietary and lifestyle changes, we can help you. We will "hold your hand" through the changes, step by step, to make each step an easy one. We are located in Clearwater, FL, at 1000 S Ft Harrison, at the corner of Ft. Harrison Ave. and Magnolia St. There is plenty of parking space directly accessible from Ft Harrison. If it is not convenient for you to come to Root Cause Medical Clinic, we offer telehealth/telemedicine consultations to residents of certain states. Call us for details.
Contact us for a Consultation – Call 727-335-0400

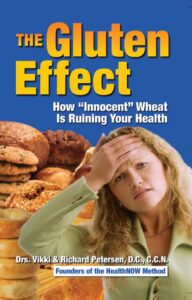
Dr. Vikki Petersen DC. CCN
Founder of Root Cause Medical Clinic
Certified Functional Medicine Practitioner
Dr Vikki Petersen is a public speaker, author of two books, several eBooks and creates cutting edge content for her YouTube community. Dr Vikki is committed to bringing Root Cause Medicine and its unique approach to restoring health naturally to the world.
Ask a Doctor
Have a health concern you'd like to speak with a doctor about? Or just want clarity on a subject? Ask Us!


