How to Fix Your Frozen Shoulder
Over 6 Million Americans Suffer
Frozen shoulder, also known as Adhesive Capsulitis, is a condition that affects around 2% of the general population. That translates to roughly 6.3 million people in America suffering from this painful condition. Our Root Cause Medical Clinic sees many patients with this condition as well.
As the name suggests, a frozen shoulder presents a decreased range of motion, pain, and stiffness of the shoulder. To understand the mechanism of this condition one must understand a little about the anatomy of the shoulder.
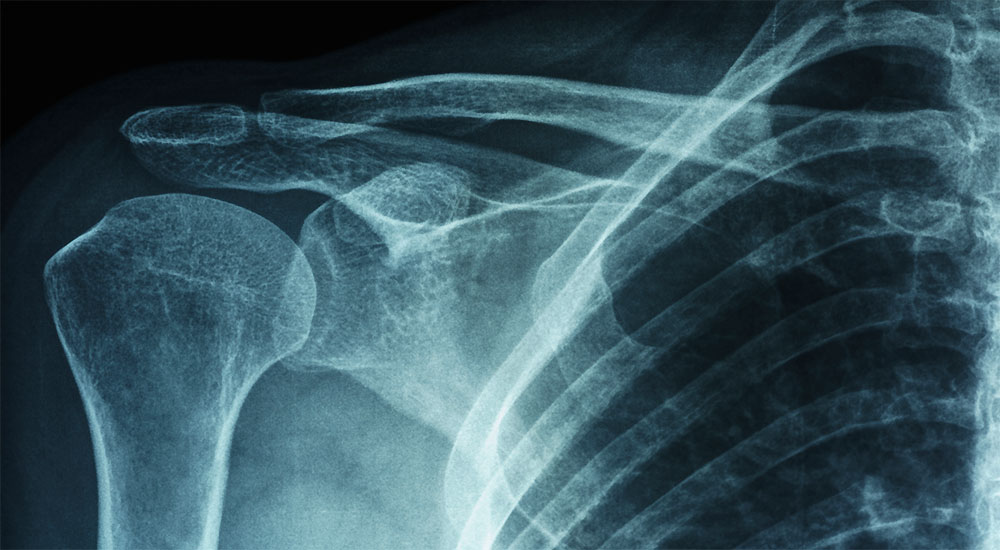
Anatomy of the Shoulder
The shoulder is comprised of three bones: the upper arm bone (humerus), the shoulder blade (scapula), and the collarbone (clavicle). These three bones form the shoulder joint which is a ball and socket joint, like your hip.
The three bones are held in place by a group of muscles called the rotator cuff muscles. A layer of connective tissues surrounds this muscle group. This connective tissue is referred to as the joint capsule.
Within the joint capsule is fluid (called synovial fluid) which acts as a lubricating agent so the humerus slides smoothly within the joint.
How Do You Know if You Have Frozen Shoulder?
With a frozen shoulder, the connective tissue surrounding the joint, the joint capsule, becomes inflamed, thickens, and becomes stiff. Adhesions develop within the connective tissue and cause the shoulder to become even tighter. The synovial fluid, or a joint lubricator, can also be diminished, in some cases, which creates more resistance to movement within the joint.
The major symptoms of frozen shoulder are:
• immobility of the shoulder
• decreased range of motion
• pain with motion
• stiffness
Frozen Shoulder, Like the Icebergs, Creep up on You Slowly
The frozen shoulder does not have an immediate severe onset, it develops in stages. The 3 stages of frozen shoulder are:
Freezing
Pain is the telltale sign of this stage. Pain starts to build in the shoulder and as the pain increases, the range of motion decreases. This stage can last from 6 weeks-9 months.
Frozen
The pain stabilizes in this stage and starts to reduce somewhat, however, the stiffness and decreased range of motion that has developed remains at that same level. This stage can last from 4-6 months and during this time routine functions such as getting dressed, brushing your teeth, and washing your hair can be difficult.
Thawing
During this stage mobility of the shoulder slowly returns. Pain continues to reduce and activities become easier as the range of motion improves. This stage normally lasts 6 months to 2 years.
What Causes Frozen Shoulder?
While research studies haven’t produced a singular causative factor that leads to frozen shoulder, they have uncovered some relationships between the frozen shoulder and the types of patients who develop it.
Here’s the list:
Age – Frozen shoulder is most commonly seen in patients ages 40-70.
Surgery/Injury – Cases in which patients have recently suffered an injury or have had surgery in the shoulder area and do not regain full range of motion afterward are at risk for developing a frozen shoulder.
Common shoulder injuries include rotator cuff tears and broken bones in the shoulder area.
Disease – Diabetes, hyper and hypothyroidism, cardiovascular disease, tuberculosis, and Parkinson’s disease have all been linked with frozen shoulder.
Gender – Women tend to develop a frozen shoulder more than men.
Inactivity – Doctors believe that prolonged immobilization of the shoulder can lead to a frozen shoulder.
Treating Frozen Shoulder
The primary goals of treatment for frozen shoulder are pain management and increased range of motion. Applying ice to the shoulder and using over the counter anti-inflammatory drugs, such as ibuprofen, can be used to reduce inflammation in the joint capsule, but are not an effective course of treatment alone. The most effective course of treatment for frozen shoulder is one that combines anti-inflammatory agents (these can be natural and our Clinical Nutrition department works with natural anti-inflammatory agents with our patients) with our Root Cause Medical Clinic.
Decreasing the inflammation in the joint capsule increases the ability of the shoulder bones to move. This allows for better success of the physical therapy techniques we utilize such as joint mobilizations, manual therapy, and therapeutic exercises.
Joint mobilizations and manual therapy, in conjunction with therapeutic exercises, have been proven to be effective at increasing range of motion. When a joint is mobilized, synovial fluid is created which makes it easier for the bones to glide in the joint socket.
Manual therapy breaks up adhesions that form in the muscles, making the muscles more flexible and allowing for better circulation throughout the area.
Severe Cases May Require Drugs or Surgery
In some cases, the inflammation of the joint capsule is so significant that over-the-counter anti-inflammatory drugs and cold therapy are insufficient to adequately decrease the inflammation. In these cases, a doctor can inject cortisone, a powerful anti-inflammatory steroid, directly into the shoulder. Following a cortisone injection, the patient can then resume the same treatment plan.
Cortisone injections, although effective, only last a few weeks and do have side effects, so they are not a permanent solution and should only be used as a last resort. Some cases are so severe that physical therapy and steroids are not successful at restoring range of motion. In these cases, a doctor may recommend surgery or manipulation under anesthesia.
Manipulation is a technique used by doctors to forcefully increase the shoulder’s range of motion. The patient is placed under anesthesia while the doctor manually forces the shoulder through its full range. This process stretches and tears the scar tissue that has formed in the shoulder. The goal of this technique is to break up scar tissue and adhesions so that the shoulder can move more freely.
Shoulder Arthroscopy is a surgical technique used to cut out scar tissue that has formed in the shoulder. With the scar tissue removed, the bones can move more freely in the joint. With both procedures, physical therapy rehabilitation is required afterward to maintain a full range of motion.
The rehabilitation process can take anywhere from a few weeks to a year. The good news is that once the full range is restored, frozen shoulder generally does not come back, as long as the shoulder remains mobile and stretches are continued. Frozen shoulder is a long, arduous process that takes a long time to get over.
If you fall into any of the at-risk categories listed above, feel pain or restricted range of motion in your shoulder, you should meet with your doctor immediately to have your shoulder examined.
We Tailor a Treatment Program to You
Here at Root Cause Medical Clinic, our Physical Therapy Department is highly experienced in treating patients with frozen shoulder. In conjunction with a variety of therapies, a customized exercise and stretching program is designed for each patient ensuring that flexibility goals are achieved with each session until a full range of motion is restored.
Do you need help with your health?
We have the diagnostic and testing tools, the clinical experience, and a different medical approach to discovering the root cause of why you have the symptoms that are bothering you. As long as you are ready to make some dietary and lifestyle changes, we can help you. We will "hold your hand" through the changes, step by step, to make each step an easy one. We are located in Clearwater, FL, at 1000 S Ft Harrison, at the corner of Ft. Harrison Ave. and Magnolia St. There is plenty of parking space directly accessible from Ft Harrison. If it is not convenient for you to come to Root Cause Medical Clinic, we offer telehealth/telemedicine consultations to residents of certain states. Call us for details.
Contact us for a Consultation – Call 727-335-0400
Ask a Doctor
Have a health concern you'd like to speak with a doctor about? Or just want clarity on a subject? Ask Us!
Featured Articles
Popular Stories

Dr. Rupa Chakravarty DPT, OCS
Director of Physical Therapy at Root Cause Medical
Doctor of Physical Therapy, Orthopedic Certified Specialist
Dr. Chakravarty has numerous certifications for different techniques in Physical Therapy practice. She employs an extensive array of manual as well as exercise techniques to manage her patients’ symptoms during their course of therapy.